Journal of Traditional Chinese Medicine ›› 2024, Vol. 44 ›› Issue (3): 564-571.DOI: 10.19852/j.cnki.jtcm.20240308.003
• Original articles • Previous Articles Next Articles
Study on blood pressure rhythm in hypertensive patients with Yin deficiency syndrome and a random forest model for predicting hypertension with Yin deficiency syndrome
ZHOU Ying1, LI Ping2, LUAN Jianwei2, SHEN Rui2, WU Yinglan2, XU Qiwen2, WANG Xinyue2, ZHU Yao2, XU Xiangru4, LIU Zitian2, JIANG Yuning2, ZHONG Yong5, HE Yun3( ), JIANG Weimin2(
), JIANG Weimin2( )
)
- 1 Department of Cardiology, the Affiliated Hospital of Nanjing University of Chinese Medicine, Jiangsu Province Hospital of Traditional Chinese Medicine, Nanjing 210029, China; Department of Health Management Centre, Jinling Hospital, Affiliated Hospital of Medical School, Nanjing University, Nanjing 210002, China
2 Department of Cardiology, the Affiliated Hospital of Nanjing University of Chinese Medicine, Jiangsu Province Hospital of Traditional Chinese Medicine, Nanjing 210029, China
3 Department of General Internal Medicine, the Affiliated Hospital of Nanjing University of Chinese Medicine, Jiangsu Province Hospital of Traditional Chinese Medicine, Nanjing 210029, China
4 Emergency Department, Longhua Hospital, Shanghai University of Traditional Chinese Medicine, Shanghai 200032, China
5 Department of Health Management Centre, Jinling Hospital, Affiliated Hospital of Medical School, Nanjing University, Nanjing 210002, China
-
Received:2023-02-22Accepted:2023-05-19Online:2024-06-15Published:2024-03-08 -
Contact:Prof. JIANG Weimin, Department of Cardiology, the Affiliated Hospital of Nanjing University of Chinese Medicine, Jiangsu Province Hospital of Traditional Chinese Medicine, Nanjing 210029, China.Jwm0410@njucm.edu.cn ; HE Yun, General Medicine Department, the Affiliated Hospital of Nanjing University of Chinese Medicine, Jiangsu Province Hospital of Traditional Chinese Medicine, Nanjing 210029, China.heyunxinxueguan@163.com Telephone: +86-25-86617147 -
Supported by:National Key R&D Program of China Project: Study on Syndrome Differentiation Standard of Yin deficiency Syndrome in Hypertension(2018YFC1704403);National Key R&D Program of China Project: Systematic Study on the Standard of Syndrome Differentiation of Yin Deficiency Syndrome(2018YFC1704400);Natural Science Foundation of Jiangsu Province: Exploring the Cardioprotective Effect and Mechanism of Qinggan Zishen Formula on Obesity and Hypertension Based on Nrf2 Regulation of Cardiac Homeostasis(BK20221422);Natural Science Foundation of Jiangsu Province: Mechanism Study on the Promotion of Cardiac Energy Metabolism Balance and Inhibition of DOX Induced Heart Failure through Nr1d1/Nfil3 Mediated Circadian Pathway by Yiqi Wenyang Formula(BK20220739)
Cite this article
ZHOU Ying, LI Ping, LUAN Jianwei, SHEN Rui, WU Yinglan, XU Qiwen, WANG Xinyue, ZHU Yao, XU Xiangru, LIU Zitian, JIANG Yuning, ZHONG Yong, HE Yun, JIANG Weimin. Study on blood pressure rhythm in hypertensive patients with Yin deficiency syndrome and a random forest model for predicting hypertension with Yin deficiency syndrome[J]. Journal of Traditional Chinese Medicine, 2024, 44(3): 564-571.
share this article
| Characteristic | Total sample (n = 234) | YX (n = 74) | NYX (n = 160) | t/χ2/F value | P value |
|---|---|---|---|---|---|
| Gender (Male/Female, n) | 154/80 | 39/35 | 115/45 | 8.266 | 0.004 |
| Age (years) | 45±11 | 47±12 | 43±11 | -2.804 | 0.005 |
| Course (mouth) | 9 (1-24) | 11 (1-36) | 6 (0-24) | -1.171 | 0.242 |
| Waist (cm) | 91±9 | 87±9 | 93±9 | 4.712 | <0.001 |
| BMI (kg/m2) | 26±3 | 25±3 | 27±3 | 4.075 | <0.001 |
| SBP (mm Hg) | 147±16 | 146±15 | 148±16 | 0.927 | 0.355 |
| DBP (mm Hg) | 94±12 | 91±14 | 95±12 | 2.358 | 0.019 |
| Heart rate (bpm) | 81±10 | 82±11 | 81±10 | -1.026 | 0.306 |
| Smoking (yes/no) | 53/181 | 8/66 | 45/115 | 8.658 | 0.003 |
| Drinking (yes/no) | 41/193 | 7/67 | 34/126 | 4.867 | 0.027 |
Table 1 General clinical characteristics in tow groups
| Characteristic | Total sample (n = 234) | YX (n = 74) | NYX (n = 160) | t/χ2/F value | P value |
|---|---|---|---|---|---|
| Gender (Male/Female, n) | 154/80 | 39/35 | 115/45 | 8.266 | 0.004 |
| Age (years) | 45±11 | 47±12 | 43±11 | -2.804 | 0.005 |
| Course (mouth) | 9 (1-24) | 11 (1-36) | 6 (0-24) | -1.171 | 0.242 |
| Waist (cm) | 91±9 | 87±9 | 93±9 | 4.712 | <0.001 |
| BMI (kg/m2) | 26±3 | 25±3 | 27±3 | 4.075 | <0.001 |
| SBP (mm Hg) | 147±16 | 146±15 | 148±16 | 0.927 | 0.355 |
| DBP (mm Hg) | 94±12 | 91±14 | 95±12 | 2.358 | 0.019 |
| Heart rate (bpm) | 81±10 | 82±11 | 81±10 | -1.026 | 0.306 |
| Smoking (yes/no) | 53/181 | 8/66 | 45/115 | 8.658 | 0.003 |
| Drinking (yes/no) | 41/193 | 7/67 | 34/126 | 4.867 | 0.027 |
| Characteristic | Total sample (n = 234) | YX (n = 74) | NYX (n = 160) | t/χ2/F value | P value |
|---|---|---|---|---|---|
| 24SBP (mm Hg) | 131.8±13.8 | 130.2±12.6 | 132.6±14.3 | 1.226 | 0.222 |
| dSBP (mm Hg) | 134.7±14.2 | 133.1±13.1 | 135.5±14.7 | 1.179 | 0.240 |
| nSBP (mm Hg) | 122.0±14.6 | 120.5±13.1 | 122.7±15.2 | 1.075 | 0.283 |
| 24DBP (mm Hg) | 83.2±11.4 | 81.2±11.0 | 84.2±11.5 | 1.871 | 0.063 |
| dDBP (mm Hg) | 85.6±11.9 | 83.4±11.5 | 86.6±12.0 | 1.882 | 0.061 |
| nDBP (mm Hg) | 75.±11.2 | 73.8±10.5 | 76.2±11.5 | 1.515 | 0.131 |
| 24MAP (mm Hg) | 99.4±11.6 | 97.5±10.9 | 100.3±11.9 | 1.702 | 0.090 |
| dMAP (mm Hg) | 102.0±12.1 | 100.0±11.3 | 102.9±12.4 | 1.692 | 0.092 |
| nMAP (mm Hg) | 91.0±11.8 | 89.4±10.8 | 91.7±12.2 | 1.399 | 0.163 |
| 24SBPSD (mm Hg) | 13.7±3.2 | 13.5±3.5 | 13.7±3.1 | 0.610 | 0.543 |
| 24DBPSD (mm Hg) | 10.7±2.4 | 10.2±2.4 | 11.0±2.5 | 2.171 | 0.031 |
| dSBPSD (mm Hg) | 12.4±3.3 | 12.4±3.3 | 12.4±3.3 | -0.055 | 0.956 |
| dDBPSD (mm Hg) | 9.7±2.7 | 9.4±2.4 | 9.8±2.8 | 1.129 | 0.260 |
| nSBPSD (mm Hg) | 10.8±3.6 | 10.4±3.7 | 11.0±3.6 | 1.254 | 0.211 |
| nDBPSD (mm Hg) | 8.7±2.9 | 7.9±2.4 | 9.0±3.0 | 2.648 | 0.009 |
| 24SBPCV (%) | 10.4±2.4 | 10.4±2.7 | 10.4±2.2 | 0.126 | 0.900 |
| 24DBPCV (%) | 13.0±3.0 | 12.7±3.2 | 13.1±2.9 | 0.949 | 0.344 |
| dSBPCV (%) | 10.1±2.2 | 10.1±2.5 | 10.1±2.1 | 0.185 | 0.853 |
| nSBPCV (%) | 12.6±2.8 | 12.4±2.9 | 12.8±2.7 | 1.012 | 0.313 |
| dDBPCV (%) | 11.3±3.0 | 11.3±3.6 | 11.32±2.8 | -0.002 | 0.998 |
| nDBPCV (%) | 14.5±4.1 | 14.2±4.6 | 14.7±3.8 | 0.794 | 0.428 |
| Circadian rhythm of BP | 9.919 | 0.019 | |||
| Dipper [n (%)] | 88 (37.6) | 22 (29.7) | 66 (41.3) | 22 | <0.001 |
| Non-dipper [n (%)] | 113 (48.3) | 41 (55.4) | 72 (45.0) | 8.504 | 0.004 |
| Riser [n (%)] | 21 (9.0) | 4 (5.4) | 17 (10.6) | 8.048 | 0.005 |
| Extreme-dipper [n (%)] | 12 (5.1) | 7 (9.5) | 5 (3.1) | 0.333 | 0.564 |
Table 2 ABPM characteristics in two groups
| Characteristic | Total sample (n = 234) | YX (n = 74) | NYX (n = 160) | t/χ2/F value | P value |
|---|---|---|---|---|---|
| 24SBP (mm Hg) | 131.8±13.8 | 130.2±12.6 | 132.6±14.3 | 1.226 | 0.222 |
| dSBP (mm Hg) | 134.7±14.2 | 133.1±13.1 | 135.5±14.7 | 1.179 | 0.240 |
| nSBP (mm Hg) | 122.0±14.6 | 120.5±13.1 | 122.7±15.2 | 1.075 | 0.283 |
| 24DBP (mm Hg) | 83.2±11.4 | 81.2±11.0 | 84.2±11.5 | 1.871 | 0.063 |
| dDBP (mm Hg) | 85.6±11.9 | 83.4±11.5 | 86.6±12.0 | 1.882 | 0.061 |
| nDBP (mm Hg) | 75.±11.2 | 73.8±10.5 | 76.2±11.5 | 1.515 | 0.131 |
| 24MAP (mm Hg) | 99.4±11.6 | 97.5±10.9 | 100.3±11.9 | 1.702 | 0.090 |
| dMAP (mm Hg) | 102.0±12.1 | 100.0±11.3 | 102.9±12.4 | 1.692 | 0.092 |
| nMAP (mm Hg) | 91.0±11.8 | 89.4±10.8 | 91.7±12.2 | 1.399 | 0.163 |
| 24SBPSD (mm Hg) | 13.7±3.2 | 13.5±3.5 | 13.7±3.1 | 0.610 | 0.543 |
| 24DBPSD (mm Hg) | 10.7±2.4 | 10.2±2.4 | 11.0±2.5 | 2.171 | 0.031 |
| dSBPSD (mm Hg) | 12.4±3.3 | 12.4±3.3 | 12.4±3.3 | -0.055 | 0.956 |
| dDBPSD (mm Hg) | 9.7±2.7 | 9.4±2.4 | 9.8±2.8 | 1.129 | 0.260 |
| nSBPSD (mm Hg) | 10.8±3.6 | 10.4±3.7 | 11.0±3.6 | 1.254 | 0.211 |
| nDBPSD (mm Hg) | 8.7±2.9 | 7.9±2.4 | 9.0±3.0 | 2.648 | 0.009 |
| 24SBPCV (%) | 10.4±2.4 | 10.4±2.7 | 10.4±2.2 | 0.126 | 0.900 |
| 24DBPCV (%) | 13.0±3.0 | 12.7±3.2 | 13.1±2.9 | 0.949 | 0.344 |
| dSBPCV (%) | 10.1±2.2 | 10.1±2.5 | 10.1±2.1 | 0.185 | 0.853 |
| nSBPCV (%) | 12.6±2.8 | 12.4±2.9 | 12.8±2.7 | 1.012 | 0.313 |
| dDBPCV (%) | 11.3±3.0 | 11.3±3.6 | 11.32±2.8 | -0.002 | 0.998 |
| nDBPCV (%) | 14.5±4.1 | 14.2±4.6 | 14.7±3.8 | 0.794 | 0.428 |
| Circadian rhythm of BP | 9.919 | 0.019 | |||
| Dipper [n (%)] | 88 (37.6) | 22 (29.7) | 66 (41.3) | 22 | <0.001 |
| Non-dipper [n (%)] | 113 (48.3) | 41 (55.4) | 72 (45.0) | 8.504 | 0.004 |
| Riser [n (%)] | 21 (9.0) | 4 (5.4) | 17 (10.6) | 8.048 | 0.005 |
| Extreme-dipper [n (%)] | 12 (5.1) | 7 (9.5) | 5 (3.1) | 0.333 | 0.564 |
| Characteristic (mm Hg) | YX (n = 74) | NYX (n = 160) | t value | P value |
|---|---|---|---|---|
| Si-Shi DBP | 88±12.6 | 91±13 | -2.183 | 0.029 |
| Si-Shi MAP | 104±12 | 107±13 | -2.105 | 0.035 |
| Hai-Shi SBP | 128±16 | 134±18 | -2.644 | 0.008 |
| Hai-Shi DBP | 78±14 | 85±15 | -3.079 | 0.002 |
| Hai-Shi MAP | 95±14 | 101±15 | 2.978 | 0.003 |
| Zi-Shi SBP | 120±15 | 125±18 | 2.188 | 0.030 |
| Zi-Shi DBP | 72±12 | 77±13 | 2.424 | 0.016 |
| Zi-Shi MAP | 88±12 | 93±14 | 2.588 | 0.011 |
| Chou-Shi SSD | 6±4 | 7±4 | -2.423 | 0.015 |
| Chou-Shi DSD | 5±3 | 6±3 | -2.214 | 0.027 |
| Chou-Shi SCV | 6±5 | 8±5 | -2.207 | 0.027 |
Table 3 ABPM characteristics of 12 two-hour periods in two groups
| Characteristic (mm Hg) | YX (n = 74) | NYX (n = 160) | t value | P value |
|---|---|---|---|---|
| Si-Shi DBP | 88±12.6 | 91±13 | -2.183 | 0.029 |
| Si-Shi MAP | 104±12 | 107±13 | -2.105 | 0.035 |
| Hai-Shi SBP | 128±16 | 134±18 | -2.644 | 0.008 |
| Hai-Shi DBP | 78±14 | 85±15 | -3.079 | 0.002 |
| Hai-Shi MAP | 95±14 | 101±15 | 2.978 | 0.003 |
| Zi-Shi SBP | 120±15 | 125±18 | 2.188 | 0.030 |
| Zi-Shi DBP | 72±12 | 77±13 | 2.424 | 0.016 |
| Zi-Shi MAP | 88±12 | 93±14 | 2.588 | 0.011 |
| Chou-Shi SSD | 6±4 | 7±4 | -2.423 | 0.015 |
| Chou-Shi DSD | 5±3 | 6±3 | -2.214 | 0.027 |
| Chou-Shi SCV | 6±5 | 8±5 | -2.207 | 0.027 |
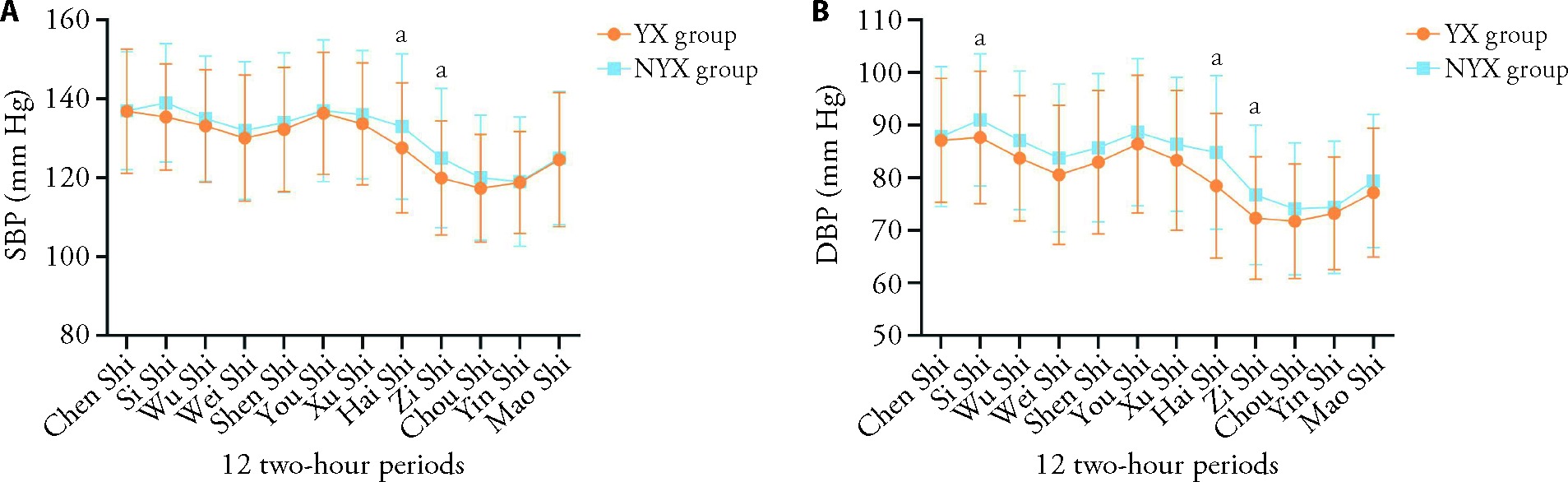
Figure 1 Mean blood pressure of 12 two-hour periods in two groups A: comparison of systolic blood pressure of 12 two-hour periods between Yin deficiency group and non-Yin deficiency group. B: comparison of diastolic blood pressure of 12 two-hour periods between Yin deficiency group and non-Yin deficiency group. Participants were grouped into Yin deficiency group (YX, n = 74) and non-Yin deficiency group (NYX, n = 140) by three experienced chief TCM physicians according to four examinations. YX: Yin deficiency; NYX: non-Yin deficiency; SBP: systolic blood pressure; DBP: diastolic blood pressure. Independent sample t-test was used for comparison between groups. Significant differences were designated as aP < 0.05.
| Characteristic | b | SE | Wald | P value | OR | 95% CI |
|---|---|---|---|---|---|---|
| Szxr | 0.156 | 0.049 | 10.159 | 0.001 | 1.169 | 1.062-1.287 |
| Ty | 0.095 | 0.052 | 3.302 | 0.069 | 1.100 | 0.993-1.219 |
| Lmgs | - | - | - | 0.124 | - | - |
| Mxx | 0.189 | 0.036 | 27.279 | <0.001 | 1.208 | 1.125-1.297 |
| Ystr | 0.268 | 0.102 | 6.919 | 0.009 | 1.307 | 1.071-1.595 |
| Mx | - | - | - | 0.477 | - | - |
| Xj | - | - | - | 0.213 | - | - |
| Qh | 0.176 | 0.050 | 12.233 | <0.001 | 1.192 | 1.080-1.315 |
| Em | - | - | - | 0.219 | - | - |
| Md | - | - | - | 0.125 | - | - |
Table 4 Binary logistic regression of TCM symptoms and diagnosis of Yin deficiency syndrome
| Characteristic | b | SE | Wald | P value | OR | 95% CI |
|---|---|---|---|---|---|---|
| Szxr | 0.156 | 0.049 | 10.159 | 0.001 | 1.169 | 1.062-1.287 |
| Ty | 0.095 | 0.052 | 3.302 | 0.069 | 1.100 | 0.993-1.219 |
| Lmgs | - | - | - | 0.124 | - | - |
| Mxx | 0.189 | 0.036 | 27.279 | <0.001 | 1.208 | 1.125-1.297 |
| Ystr | 0.268 | 0.102 | 6.919 | 0.009 | 1.307 | 1.071-1.595 |
| Mx | - | - | - | 0.477 | - | - |
| Xj | - | - | - | 0.213 | - | - |
| Qh | 0.176 | 0.050 | 12.233 | <0.001 | 1.192 | 1.080-1.315 |
| Em | - | - | - | 0.219 | - | - |
| Md | - | - | - | 0.125 | - | - |
| Characteristic | b | SE | Wald | P | OR | 95% CI |
|---|---|---|---|---|---|---|
| 24SBPCV | -1.587 | 0.685 | 5.360 | 0.021 | 0.205 | 0.053-0.784 |
| dSBPSD | 0.529 | 0.177 | 8.916 | 0.003 | 1.697 | 1.199-2.402 |
| dDBPSD | -0.190 | 0.09 | 4.506 | 0.034 | 0.827 | 0.693-0.986 |
| nSBPSD | 0.147 | 0.072 | 4.156 | 0.041 | 1.158 | 1.006-1.334 |
| nSBPCV | 0.993 | 0.434 | 5.238 | 0.022 | 2.699 | 1.153-6.317 |
| nDBPSD | -0.204 | 0.077 | 7.002 | 0.008 | 0.815 | 0.701-0.948 |
| Hai-Shi DBP | -0.051 | 0.025 | 4.262 | 0.039 | 0.950 | 0.906-0.997 |
| Hai-Shi SCV | 0.104 | 0.052 | 3.941 | 0.047 | 1.109 | 1.001-1.229 |
Table 5 Binary Logistic Regression of BPV and diagnosis of Yin Deficiency Syndrome
| Characteristic | b | SE | Wald | P | OR | 95% CI |
|---|---|---|---|---|---|---|
| 24SBPCV | -1.587 | 0.685 | 5.360 | 0.021 | 0.205 | 0.053-0.784 |
| dSBPSD | 0.529 | 0.177 | 8.916 | 0.003 | 1.697 | 1.199-2.402 |
| dDBPSD | -0.190 | 0.09 | 4.506 | 0.034 | 0.827 | 0.693-0.986 |
| nSBPSD | 0.147 | 0.072 | 4.156 | 0.041 | 1.158 | 1.006-1.334 |
| nSBPCV | 0.993 | 0.434 | 5.238 | 0.022 | 2.699 | 1.153-6.317 |
| nDBPSD | -0.204 | 0.077 | 7.002 | 0.008 | 0.815 | 0.701-0.948 |
| Hai-Shi DBP | -0.051 | 0.025 | 4.262 | 0.039 | 0.950 | 0.906-0.997 |
| Hai-Shi SCV | 0.104 | 0.052 | 3.941 | 0.047 | 1.109 | 1.001-1.229 |
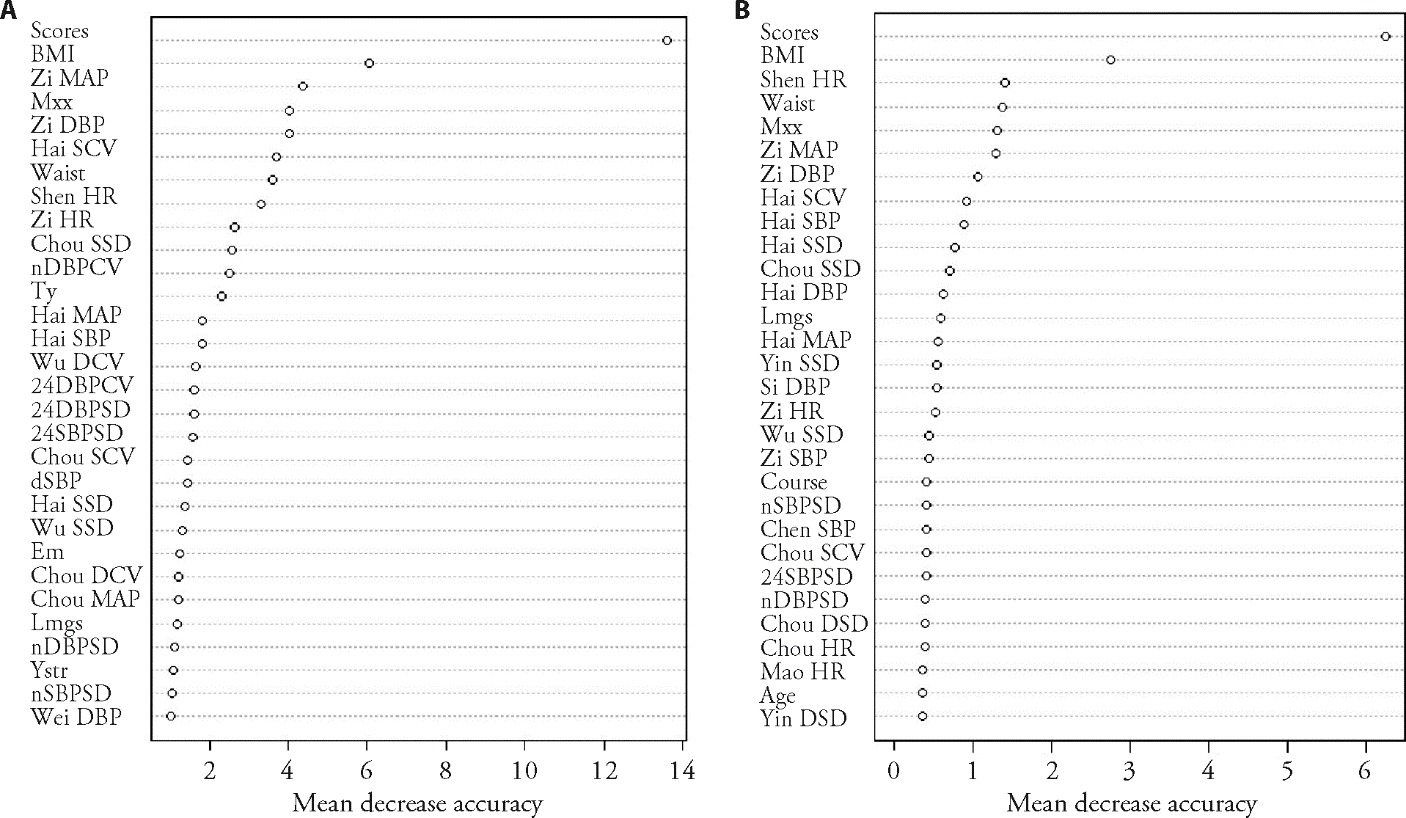
Figure 2 Mean decrease in accuracy and mean decrease in Gini A: the influencing indicators of Yin deficiency syndrome of hypertension were ordered according to the mean decrease accuracy index. B: the influencing indicators of Yin deficiency syndrome of hypertension were ordered according to the mean decrease Gini index. It refers to the degree of decrease in accuracy without the presence of this diagnostic indicator in the random forest model, which is equivalent to the concept of classification contribution. The higher the value, the more important the contribution. Scores: scores of Yin deficiency syndrome of hypertension rating scale; BMI: body mass index; SBP: systolic blood pressure; DBP: diastolic blood pressure; MBP: mean arterial pressure; Zi MBP: Zi-Shi mean arterial pressure; Mxx: string-like and fine pulse; Zi DBP: Zi-Shi diastolic blood pressure; Hai SCV: Hai-Shi SBP coefficient of variation; Waist: waist circumference; Shen HR: Shen-Shi heart rate; Zi HR: Zi-Shi heart rate; Chou SSD: Chou-Shi SBP standard deviation; nDBPCV: nighttime DBP coefficient of variation; Ty: dizziness; Hai MBP: Hai-Shi mean arterial pressure; Hai SBP: Hai-Shi systolic blood pressure; Wu DCV: Wu-Shi DBP coefficient of variation; 24DBPCV: 24 h DBP coefficient of variation; 24DBPSD: 24 h DBP standard deviation; 24SBPSD: 24 h SBP standard deviation; Chou SCV: Chou-Shi SBP coefficient of variation; dSBP: daytime SBP; Hai SSD: Hai-Shi SBP standard deviation; Wu SSD: Wu-Shi SBP standard deviation; Em: tinnitus; Chou DCV: Chou-Shi DBP coefficient of variation; Chou MBP: Chou-Shi mean arterial pressure; Lmgs: dry eyes; nDBPSD: nighttime DBP standard deviation; Ystr: soreness and weakness of lumbus and knees; Wei DBP: Wei-Shi diastolic blood pressure; Hai DBP: Hai-Shi diastolic blood pressure; Yin SSD: Yin-Shi SBP standard deviation; Si DBP: Si-Shi diastolic blood pressure; Course: course of hypertension; Chen SBP: Chen-Shi systolic blood pressure; Chou DSD: Chou-Shi DBP standard deviation; Chou HR: Chou-Shi heart rate; Mao HR: Mao-Shi heart rate; Yin DSD: Yin-Shi DBP standard deviation.
| 1. |
Kuhlman SJ, Craig LM, Duffy JF. Introduction to chronobiology. Cold Spring Harb Perspect Biol 2018; 10: a033613.
DOI URL |
| 2. |
Costello HM, Gumz ML. Circadian rhythm, clock genes, and hypertension: recent advances in hypertension. Hypertension 2021; 78: 1185-96.
DOI URL |
| 3. |
Smolensky MH, Hermida RC, Portaluppi F. Circadian mechanisms of 24-hour blood pressure regulation and patterning. Sleep Med Rev 2017; 33: 4-16.
DOI PMID |
| 4. |
Mehlum MH, Liestøl K, Kjeldsen SE, et al. Blood pressure variability and risk of cardiovascular events and death in patients with hypertension and different baseline risks. Eur Heart J 2018; 39: 2243-51.
DOI PMID |
| 5. |
Parati G, Torlasco C, Pengo M, et al. Blood pressure variability: its relevance for cardiovascular homeostasis and cardiovascular diseases. Hypertens Res 2020; 43: 609-20.
DOI PMID |
| 6. |
Parati G, Stergiou GS, Dolan E, et al. Blood pressure variability: clinical relevance and application. J Clin Hypertens (Greenwich) 2018; 20: 1133-7.
DOI PMID |
| 7. | Tian DH, Liu GS. Huang Di Nei Jing-Lingshu. Beijing: People's medical publishing house, 2005: 2-3. |
| 8. | Meng JX, Mao JY, Wang XL. Correlation between circadian rhythm of blood pressure and chronological regularity of meridian flow. Zhong Yi Za Zhi 2015; 56: 1378-81. |
| 9. | Liang S, Liu M, Liang JY, et al. A cross-sectional study on the structural and functional characteristics of the left ventricle in patients with hypertension with different TCM syndrome types in Danyang city, Jiangsu province. Zhong Yi Za Zhi 2022; 63: 658-63. |
| 10. |
Jackson EA, El Khoudary SR, Crawford SL, et al. Hot flash frequency and blood pressure: data from the study of women's health across the nation. J Womens Health (Larchmt) 2016; 25: 1204-9.
DOI PMID |
| 11. | Guidelines for the prevention and treatment of hypertension in China (2018 revised edition). Zhong Guo Xin Xue Guan Za Zhi 2019; 24: 24-56. |
| 12. | Zhen XY. Guidelines for clinical research of new drugs of Traditional Chinese Medicine (trial). Beijing: China Medical Science and Technology Press, 2002: 74-5. |
| 13. |
Kario K, Shin J, Chen CH, et al. Expert panel consensus recommendations for ambulatory blood pressure monitoring in Asia: the HOPE Asia Network. J Clin Hypertens (Greenwich) 2019; 21: 1250-83.
DOI PMID |
| 14. | He Y, He J, Xu XR, et al. Consensus on diagnostic criteria for deficiency syndrome in hypertension: a modified Delphi study. J Tradit Chin Med 2023; 43: 181-7. |
| 15. | Cortés-Ríos J, Rodriguez-Fernandez M. Circadian rhythm of blood pressure of dipper and non-dipper patients with essential hypertension: a mathematical modeling approach. Front Physiol 2020; 11: 536146. |
| 16. | Morris CJ, Purvis TE, Hu K, et al. Circadian misalignment increases cardiovascular disease risk factors in humans. Proc Natl Acad Sci U S A 2016; 113: E1402-11. |
| 17. |
Cuspidi C, Tadic M, Grassi G. Blood pressure variability: a new therapeutic target on the horizon. J Hypertens 2021; 39: 1771-73.
DOI PMID |
| 18. |
Asayama K, Satoh M, Kikuya M. Diurnal blood pressure changes. Hypertens Res 2018; 41: 669-78.
DOI PMID |
| 19. |
Madden JM, O'flynn AM, Fitzgerald AP, et al. Correlation between short-term blood pressure variability and left-ventricular mass index: a Meta-analysis. Hypertens Res 2016; 39: 171-7.
DOI PMID |
| 20. | Hermida RC, Crespo JJ, Domínguez-Sardiña M, et al. Bedtime hypertension treatment improves cardiovascular risk reduction: the hygia chronotherapy trial. Eur Heart J 2020; 41: 4565-76. |
| 21. | Wang Y, Sun B, Hu Y. Therapeutic effect of adjuvant treatment of acupuncture in a period of day from 7:00 am to 9:00 am on non-dipper essential hypertension. Zhong Guo Zhen Jiu Za Zhi 2020; 40: 591-5. |
| 22. | Gao X, Li X. Understanding of TCM on abnormal blood pressure rhythm. Zhong Yi Za Zhi 2016; 57: 1798-800. |
| [1] | HE Yun, HE Jing, XU Xiangru, LI Haixiao, SHI Rongwei, LIANG Junya, ZHOU Ying, ZHU Yao, CHEN Xiaohu, TANG Shuhua, XIAO Min, ZHAN Libin, PEI Yinghao, JIANG Weiming. Consensus on diagnostic criteria for Yin deficiency syndrome in hypertension: a modified Delphi study [J]. Journal of Traditional Chinese Medicine, 2023, 43(1): 181-187. |
| [2] | LIU Wei, XIONG Xingjiang, QIAO Lumin, CHEN Yuyi, LI Yixuan, SU Xing, CHU Fuyong, LIU Hongxu. Acupoint application therapies for essential hypertension: a systematic review and Meta-analysis [J]. Journal of Traditional Chinese Medicine, 2022, 42(2): 159-166. |
| [3] | ZHAO Zhiyue, SHI Zhenyu, ZHANG Zhenzhen, LI Yinghong, ZENG Xiaohui, CHEN Yuxing, YAO Nan, ZHOU Min, SU Hui, WANG Qinghai, JIN LiLi. Anti-hypertensive and endothelia protective effects of Fufang Qima capsule(复方芪麻胶囊) on primary hypertension via adiponectin/adenosine monophosphate activated protein kinase pathway [J]. Journal of Traditional Chinese Medicine, 2021, 41(6): 919-926. |
| [4] | ZHU Guohua, SUN Xipeng, DING Cuntao, ZHAO Huan, LI Jing, HUA Qi. Effect of Songlingxuemaikang(松龄血脉康) on mild essential hypertension in patients: a randomized parallel-controlled study [J]. Journal of Traditional Chinese Medicine, 2021, 41(5): 799-805. |
| [5] | An Xing, Li Songtao, Weng Xiangwen, Wang Xian, Wu Hao, Zhang Xinyue, Gao Jian, Yang Renxu, Peng Bo. Maxingxiongting mixture attenuates hypoxia pulmonary arterial hypertension to improve right ventricular hypertrophy by inhibiting the rho-kinase signaling pathway [J]. Journal of Traditional Chinese Medicine, 2020, 40(6): 992-998. |
| [6] | Bumjung Kim, Cheolmin Jo, Somin Lee, Hanna Choi, Kwang-Woo Kim, Inhye Ham, Ho-Young Choi, Kyungjin Lee. Vasorelaxant effects of 50 commonly used traditional herbal prescriptions on isolated rat aortic rings [J]. Journal of Traditional Chinese Medicine, 2020, 40(4): 629-639. |
| [7] | Pei Lixin, Shu Shengnan, Wang Xuanying, Ji Baoyu. Effect of chrysanthemum extract on myocardial fibrosis in rats with renovascular hypertension [J]. Journal of Traditional Chinese Medicine, 2019, 39(04): 542-549. |
| [8] | Vilaval Termklinchan, Sasinan Wasin, Mayuree Choesomboon, Chananun Praditbatuka, Somchai Sukareechai. Effect of acupuncture on blood pressure control in hypertensive patients [J]. Journal of Traditional Chinese Medicine, 2019, 39(02): 246-250. |
| [9] | Luo Xiaozhou, Huang Jianting, Yu Juan, Tang Chunzhi. Effect of Taichong(LR 3) acupuncture in spontaneously hypertensive rats [J]. Journal of Traditional Chinese Medicine, 2019, 39(01): 74-80. |
| [10] | Zhang Lu, Wu Lili, Liu Ximing, Yoshitomi Hisae, Ikeda Katsumi, Negishi Hiroko, Pan Yajing, Sun Wen, Qin Lingling, Li Juan-E, Xu Tunhai, Liu Tonghua, Gao Ming. Trans-cinnamaldehyde promotes nitric oxide release via the protein kinase-B/v-Akt murine thymoma viral oncogene-endothelial nitric oxide synthase pathway to alleviate hypertension in SHR.Cg-Lepr~(cp)/NDmcr rats [J]. Journal of Traditional Chinese Medicine, 2018, 38(04): 548-555. |
| [11] | Guo Qiulei, Liu Qingguo, Sun Dongmei, Nie Binbin. Twirling reinforcing-reducing manipulation——central mechanism underlying antihypertensive effect on spontaneous hypertension in rats [J]. Journal of Traditional Chinese Medicine, 2018, 38(03): 391-398. |
| [12] | Guo Yan, Lu Juan, Liang Jingrong, Zhao Ruili, Xu Jing, Zhang Wei, Park Kibeum, Zhu Shipeng, Chen Huan, Ma Liangxiao. Effect of acupuncture at Renying(ST 9) on gene expression profile of hypothalamus in spontaneously hypertensive rats [J]. Journal of Traditional Chinese Medicine, 2018, 38(02): 227-241. |
| [13] | Zhu Jie, Wang Baoqin, Liu Changan, Tong Xiangli, Li Zegeng. Qibai Pingfei capsule medicated serum inhibits the proliferation of hypoxia-induced pulmonary arterial smooth muscle cells via the Ca~(2+)/calcineurin/nuclear factor of activated T-cells 3 pathway [J]. Journal of Traditional Chinese Medicine, 2017, 37(04): 466-474. |
| [14] | Wonseok Chung, Jimi Ryu, Seokhee Chung, Sungsoo Kim. Effect of Qingxue Dan on obesity and metabolic biomarker: a double-blind randomized-controlled pilot study [J]. Journal of Traditional Chinese Medicine, 2016, 36(03): 291-298. |
| [15] | He Ling, Fang Meixia, Chen Liguo, Zhou Jianhua, Yuan Jing, Xu Jing, Shan Yan, Xu Qingyun, Xiong Tingting. Transcriptome analysis of blood stasis syndrome in subjects with hypertension [J]. Journal of Traditional Chinese Medicine, 2016, 36(02): 173-180. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||

