Journal of Traditional Chinese Medicine ›› 2025, Vol. 45 ›› Issue (1): 1-12.DOI: 10.19852/j.cnki.jtcm.2025.01.001
Hewei Jiangni granule (和胃降逆颗粒) alleviates visceral hypersensitivity of non-erosive reflux disease via stromal interaction molecule 1/transient receptor potential vanilloid subfamily member 1 pathway
CHENG Yuan1, ZHANG Xiaosi2, LI Junxiang2, ZHANG Liming2, DAI Yi2,3, XIE Chune2, SHI Lei2, LI Xiaohong2( ), KOU Fushun4(
), KOU Fushun4( )
)
- 1 School of Traditional Chinese Medicine and School of Integrated Chinese and Western Medicine, Nanjing University of Chinese Medicine, Nanjing 210023, China; Gastroenterology Department, Dongfang Hospital, Beijing University of Chinese Medicine, Beijing 100078, China
2 Gastroenterology Department, Dongfang Hospital, Beijing University of Chinese Medicine, Beijing 100078, China
3 Department of Pharmacotherapy and Oriental Medicine, School of Pharmacy, Hyogo University of Health Sciences, Hyogo 650-8530, Japan
4 Center for IBD Research, Department of Gastroenterology, Shanghai Tenth People's Hospital, Tongji University School of Medicine, Shanghai 200072, China
-
Received:2023-06-11Accepted:2023-10-22Online:2025-02-15Published:2025-01-10 -
Contact:Prof. LI Xiaohong, Gastroenterology Department, Dongfang Hospital, Beijing University of Chinese Medicine, Beijing 100078, China,lxhktxz@163.com ; Dr KOU Fushun, Center for IBD Research, Department of Gastroenterology, Shanghai Tenth People's Hospital, Tongji University School of Medicine, Shanghai 200072, China,koufushun@126.com , Telephone: +86-10-67689655; +86-25-85311836 -
Supported by:National Natural Science Foundation of China: Study on the Molecular Mechanism of the Regulation of Crypt Goblet Cell Pyroptosis and Exocytosis to Repair Ulcerative Colitis Mucus Barrier by the Method of Clearing and Opening the Xuanfu from the Perspective of "Xuanfu-Crypt"(82305143);National Natural Science Foundation of China: Exploring the Molecular Mechanism of "Hewei Jiangni Fang" Intervention in Non-erosive Reflux Disease Esophageal Hypersensitivity from the Perspective of Mas-related Gene X2/Stromal Interaction Molecule 1/Cell Adhesion Molecule 1 Pathway Regulation of Mast Cell/Dorsal Root Ganglion Communication based on the "Xinkai-Kujiang" Method(82374401)
Cite this article
CHENG Yuan, ZHANG Xiaosi, LI Junxiang, ZHANG Liming, DAI Yi, XIE Chune, SHI Lei, LI Xiaohong, KOU Fushun. Hewei Jiangni granule (和胃降逆颗粒) alleviates visceral hypersensitivity of non-erosive reflux disease via stromal interaction molecule 1/transient receptor potential vanilloid subfamily member 1 pathway[J]. Journal of Traditional Chinese Medicine, 2025, 45(1): 1-12.
share this article

Figure 1 HWJNG ameliorated pathological damage and regulated related indicators in NERD mice A: HE staining of esophageal mucosa in lower third of esophagus of mice (× 200), respectively; B: toluidine blue staining of esophageal mucosa in lower third of esophagus of mice (× 200), respectively; C: total counts of MCs; D: blood glucose; E: weights; F: PH values; G: mechanical paw withdrawal threshold; H: thermal withdrawal latency. A1, B1: Control group; A2, B2: Model group; A3, B3: Omeprazole group; A4, B4: HWJNG-L group; A5, B5: HWJNG-H group. Control group: deionized water; Model group: fructose water and restraint stress; Omeprazole group: model group + Omeprazole at 0.06 mg·kg-1·d-1; HWJNG-L: low dose of HWJNG at 0.24 g/kg; HWJNG-H: high dose of HWJNG at 0.48 g/kg. HWJNG: Hewei Jiangni granule. Statistical analyses were measured using one-way analysis of variance for multimal comparisons. Data were presented as mean ± standard deviation (n = 5). Compared with the control group, aP < 0.001, dP < 0.01; compared with the model group, bP < 0.001, eP < 0.01; compared with the HWJNG-H group, cP = 0.08, fP < 0.05.
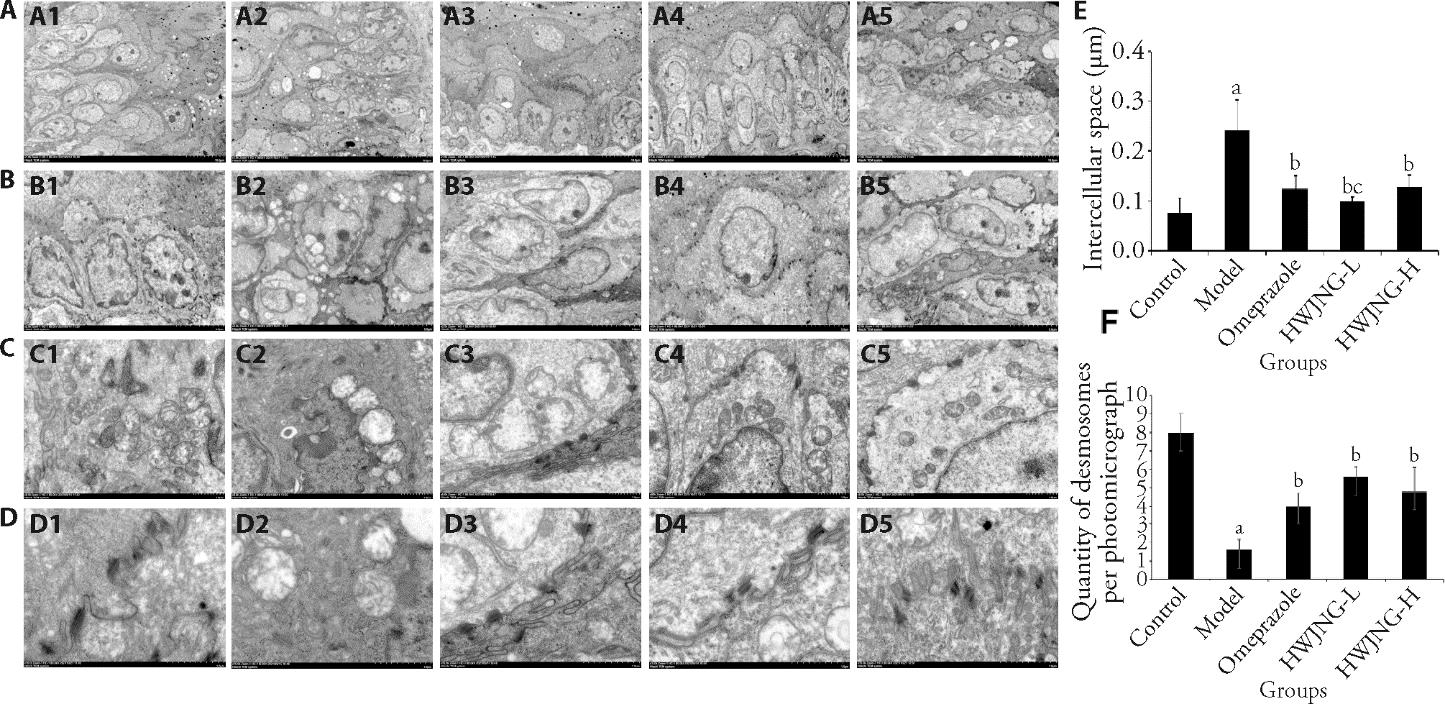
Figure 2 Observation of pathological damage in non-erosive reflux disease repaired by HWJNG under electron microscopy A: dilated epithelial cell space (× 1000); B: dilated intercellular space (× 2500); C: mitochondria morphological changes (× 8000); D: desmosome morphological changes (× 15 000); E: width of mucosal intercellular space (× 2500); F: quantity of desmosomes (× 15000). A1, B1, C1, D1: Control group; A2, B2, C2, D2: model group; A3, B3, C3, D3: omeprazole group; A4, B4, C4, D4: HWJNG-L group; A5, B5, C5, D5: HWJNG-H group. Control group: deionized water; Model group: fructose water and restraint stress; Omeprazole group: model group + Omeprazole at 0.06 mg·kg-1·d-1; HWJNG-L: low dose of HWJNG at 0.24 g/kg; HWJNG-H: high dose of HWJNG at 0.48 g/kg. HWJNG: Hewei Jiangni granule. Statistical analyses were measured using one-way analysis of variance for multimal comparisons. Data were presented as mean ± standard deviation (n = 5). Compared with the control group, aP < 0.001; compared with the model group, bP < 0.001; compared with the HWJNG-H group, cP < 0.05.
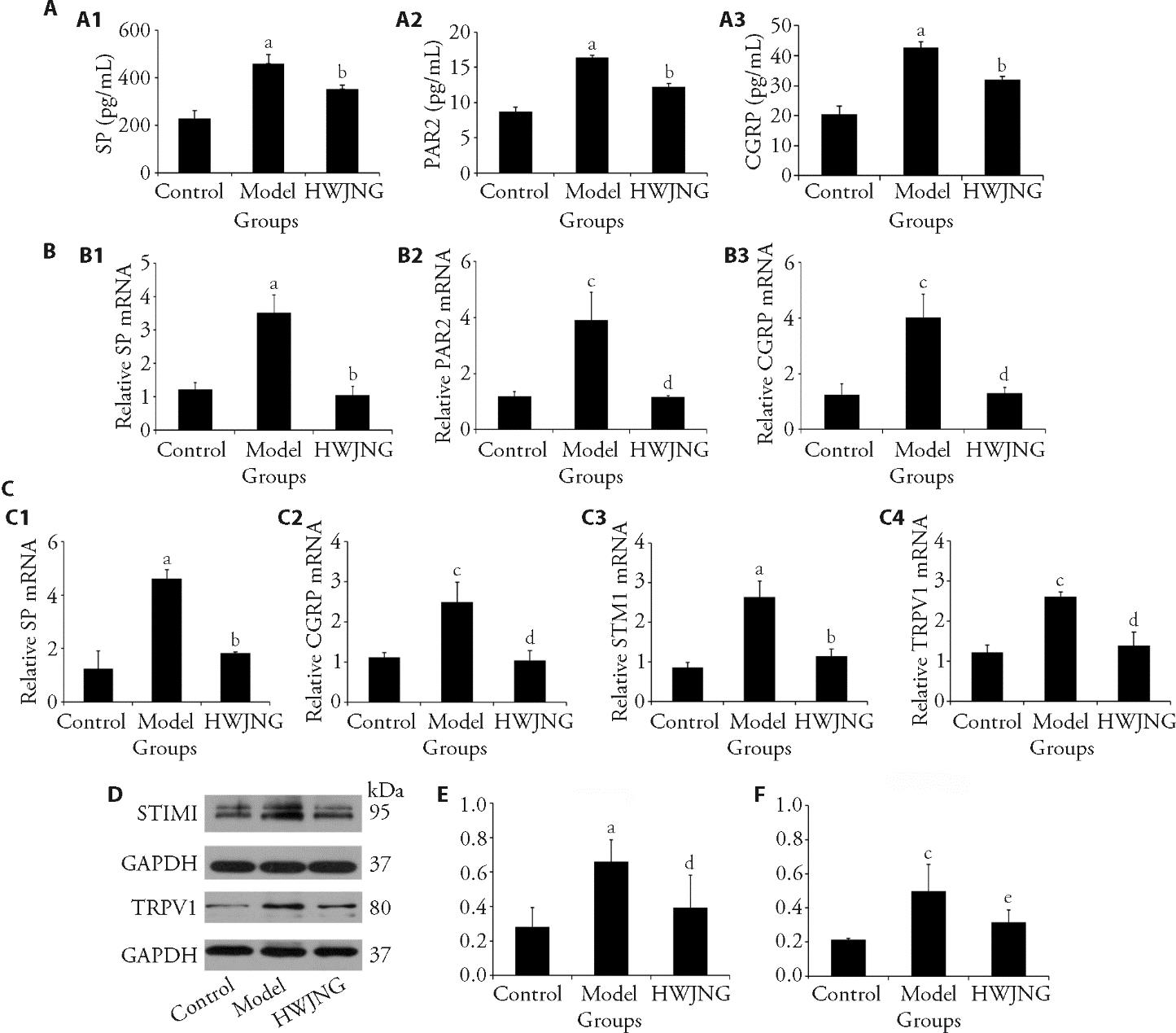
Figure 3 HWJNG treatment regulates protein and mRNA expressions of STIM1, TRPV1 and related neurotransmitters in esophageal mucosa and DRG of mice A: relative protein levels of SP, PAR2, and CGRP in esophageal mucosa (n = 5). A1: SP; A2: PAR2; A3: CGRP. B: relative m RNA levels of SP, PAR2 and CGRP assessed in esophageal mucosa (n = 3). B1: SP; B2: PAR2; B3: CGRP. C: relativemRNA levels of SP, CGRP, STIM1 and TRPV1 assessed in DRG (n = 3). C1: SP; C2: CGRP; C3: STIM1; C4: TRPV1. D: representative band of STIM1 and TRPV1 protein detected by WB in DRG (n = 3). E: relative protein levels of STIM1 results in DRG (n = 3). F: relative protein levels of TRPV1 results in DRG (n = 3). Control group: deionized water; Model group: fructose water and restraint stress; HWJNG: Low dose of HWJNG at 0.24 g/kg + high dose of HWJNG at 0.48 g/kg. STIM1: stromal interaction molecule 1; TRPV1: transient receptor potential vanilloid subfamily member 1; DRG: dorsal root ganglion cells; SP: substance P; PAR2: protease activated receptors-2; CGRP: calcitonin gene-related peptide; HWJNG: Hewei Jiangni granule. Statistical analyses were measured using one-way analysis of variance for multimal comparisons. Data were presented as mean ± standard deviation (n = 5). Compared with the control group, aP < 0.001, cP < 0.01; compared with the model group, bP < 0.001, dP < 0.01. eP < 0.05.

Figure 4 STIM1 deficiency and overexpression affect the therapeutic of HWJNG on DRG cells with P815 cells co-culture A: P815 cells adhesion to DRGs cells via a fluorescence adhesion assay in different groups. The protein levels of PAR2. A1: Blank; A2: Model; A3: model + HWJNG; A4: model + oeCtrl; A5: model + oeSTIM1 + HWJNG; A6: model + siCtrl; A7: model + siSTIM1. B: relative protein levels of SP assessed by ELISA in DRG cells. C: relative protein levels of PAR2 assessed by ELISA in DRG cells. D: relative protein levels of CGRP assessed by ELISA in DRG cells. E: levels of Orai1 mRNA assessed by RT- qPCR in DRG cells. F: levels of TRPV1 mRNA assessed by RT- qPCR in DRG cells. G: levels of STIM1 mRNA assessed by RT- qPCR in DRG cells. Blank group: DRG cells with P815 Cells; Model group: blank group + SP; Model + HWJNG: Model group + HWJNG; Model + oeCtrl: Model group + oeCtrl; Model + oeSTIM1 + HWJNG; Model group + oeSTIM1 + HWJNG; Model + siCtrl: Model group + siCtrl; Model + siSTIM1: Model group + siSTIM1; oeCtrl; STIM1 overexpression control; oeSTIMI; overexpression STIM1; siCtrl; STIM1 siRNA control; siSTIM1; siRNA STIM1. SP: substance P; STIM1: stromal interaction molecule 1; TRPV1: potential vanilloid subfamily member 1; PAR-2: protease activated receptor-2; CGRP: alcitonin gene-related peptide; HWJNG: Hewei Jiangni granule. Statistical analyses were measured using one-way analysis of variance for multimal comparisons. Data were presented as mean ± standard deviation (n = 5). Compared with the control group, aP < 0.001; compared with the model group, bP < 0.001; compared with the model + HWJNG group, cP < 0.01, dP < 0.05.
| 1. |
Richter JE, Rubenstein JH. Presentation and epidemiology of gastroesophageal reflux disease. Gastroenterology 2018; 154: 267-76.
DOI PMID |
| 2. | Katzka DA, Pandolfino JE, Kahrilas PJ. Phenotypes of gastroesophageal reflux disease: where Rome, Lyon, and Montreal meet. Clin Gastroenterol Hepatol 2020; 18: 767-76. |
| 3. |
Fass R, Boeckxstaens GE, El-Serag H, Rosen R, Sifrim D, Vaezi MF. Gastro-oesophageal reflux disease. Nat Rev Dis Primers 2021; 7: 55.
DOI PMID |
| 4. | Chapelle N, Ben Ghezala I, Barkun A, Bardou M. The pharmacotherapeutic management of gastroesophageal reflux disease (GERD). Expert Opin Pharmacother 2021; 22: 219-27. |
| 5. | Talley NJ, Zand Irani M. Optimal management of severe symptomatic gastroesophageal reflux disease. J Intern Med 2021; 289: 162-78. |
| 6. | Patel D, Fass R, Vaezi M. Untangling nonerosive reflux disease from functional heartburn. Clin Gastroenterol Hepatol 2021; 19: 1314-26. |
| 7. | Katzka DA, Kahrilas PJ. Advances in the diagnosis and management of gastroesophageal reflux disease. BMJ 2020; 371: m3786. |
| 8. | Sharma P, Yadlapati R. Pathophysiology and treatment options for gastroesophageal reflux disease: looking beyond acid. Ann N Y Acad Sci 2021; 1486: 3-14. |
| 9. | Losa M, Manz SM, Schindler V, Savarino E, Pohl D. Increased visceral sensitivity, elevated anxiety, and depression levels in patients with functional esophageal disorders and non-erosive reflux disease. Neurogastroenterol Motil 2021; 33: e14177. |
| 10. |
Bhuiyan P, Wang YW, Sha HH, Dong HQ, Qian YN. Neuroimmune connections between corticotropin-releasing hormone and mast cells: novel strategies for the treatment of neurodegenerative diseases. Neural Regen Res 2021; 16: 2184-97.
DOI PMID |
| 11. | Silva RO, Oliveira FFB, Bingana RD, et al. A novel murine model of esophageal nonerosive reflux disease: from inflammation to impairment in mucosal integrity. Am J Physiol Gastrointest Liver Physiol 2017; 312: G658-65. |
| 12. |
Voisin T, Bouvier A, Chiu IM. Neuro-immune interactions in allergic diseases: novel targets for therapeutics. Int Immunol 2017; 29: 247-61.
DOI PMID |
| 13. | Weinstock LB, Pace LA, Rezaie A, Afrin LB, Molderings GJ. Mast cell activation syndrome: a primer for the gastroenterologist. Dig Dis Sci 2021; 66: 965-82. |
| 14. |
Kamphuis JBJ, Guiard B, Leveque M, et al. Lactose and fructo-oligosaccharides increase visceral sensitivity in mice via glycation processes, increasing mast cell density in colonic mucosa. gastroenterology 2020; 158: 652-63 e6.
DOI PMID |
| 15. |
Gupta K, Harvima IT. Mast cell-neural interactions contribute to pain and itch. Immunol Rev 2018; 282: 168-87.
DOI PMID |
| 16. | Lin YP, Bakowski D, Mirams GR, Parekh AB. Selective recruitment of different Ca(2+)-dependent transcription factors by STIM1-Orai1 channel clusters. Nat Commun 2019; 10: 2516. |
| 17. | Ustaoglu A, Sawada A, Lee C, et al. Heartburn sensation in nonerosive reflux disease: pattern of superficial sensory nerves expressing TRPV1 and epithelial cells expressing ASIC 3 receptors. Am J Physiol Gastrointest Liver Physiol 2021; 320: G804-15. |
| 18. | Silva RO, Bingana RD, Sales T, et al. Role of TRPV1 receptor in inflammation and impairment of esophageal mucosal integrity in a murine model of nonerosive reflux disease. Neurogastroenterol Motil 2018: e13340. |
| 19. | Ustaoglu A, Nguyen A, Spechler S, Sifrim D, Souza R, Woodland P. Mucosal pathogenesis in gastro-esophageal reflux disease. Neurogastroenterol Motil 2020; 32: e14022. |
| 20. | Li JX. Clinical observation on 50 cases of reflux esophagitis treated with Hewei Jiangni granule. J Tradit Chin Med 2002: 675-6. |
| 21. | Yang Q, Li JX, Li XH. Effects of modified Banxia Xiexin decoction on symptoms and quality of life in non-erosive reflux disease. Beijing Zhong Yi Yao Da Xue Xue Bao 2013; 36: 280-5. |
| 22. | Cheng Y, Kou F, Zhang X, et al. Network pharmacology analysis of Hewei Jiangni granule for gastroesophageal reflux disease and experimental verification of its anti-neurogenic inflammation mechanism. Drug Des Devel Ther 2022; 16: 1349-63. |
| 23. | Huang JH, Huang XH, Chen ZY, Zheng QS, Sun RY. Dose conversion among different animals and healthy volunteers in pharmacological study. Chin J Clin Pharmacol Ther 2004; 9: 1069. |
| 24. | Wang Y, Li G, Wang X, Zhu S. Effects of Shugan Hewei granule on depressive behavior and protein expression related to visceral sensitivity in a rat model of nonerosive reflux disease. Evid Based Complement Alternat Med 2019; 2019: 1505693. |
| 25. | Wulamu W, Yisireyili M, Aili A, et al. Chronic stress augments esophageal inflammation, and alters the expression of transient receptor potential vanilloid 1 and protease‑activated receptor 2 in a murine model. Mol Med Rep 2019; 19: 5386-96. |
| 26. | Surdenikova L, Ru F, Nassenstein C, Tatar M, Kollarik M. The neural crest- and placodes-derived afferent innervation of the mouse esophagus. Neurogastroenterol Motil 2012; 24: e517-25. |
| 27. |
Lu M, Fang XX, Shi DD, et al. A selective TRPC3 inhibitor pyr3 attenuates myocardial ischemia/reperfusion injury in mice. Curr Med Sci 2020; 40: 1107-13.
DOI PMID |
| 28. |
Li Q, Kong L, Zhang S, et al. A novel external esophageal perfusion model for reflux-associated respiratory symptoms. Pathobiology 2010; 77: 163-8.
DOI PMID |
| 29. | Chaplan SR, Bach FW, Pogrel JW, Chung JM, Yaksh TL. Quantitative assessment of tactile allodynia in the rat paw. J Neurosci Methods 1994; 53: 55-63. |
| 30. | Jia BY, Xie CE, Wang ZB, et al. The effect of Heweijiangni-decoction on esophageal morphology in a rat model of OVA-induced visceral hypersensitivity followed by acid exposure. Cell Mol Biol (Noisy-le-grand) 2019; 65: 73-8. |
| 31. | Kim YS, Kim N, Kim GH. Sex and gender differences in gastroesophageal reflux disease. J Neurogastroenterol Motil 2016; 22: 575-88. |
| 32. | Nikaki K, Woodland P, Lee C, et al. Esophageal mucosal innervation in functional heartburn: closer to healthy asymptomatic subjects than to non-erosive reflux disease patients. Neurogastroenterol Motil 2019; 31: e13667. |
| 33. | Zayachkivska O, Havryluk O, Hrycevych N, Bula N, Grushka O, Wallace JL. Cytoprotective effects of hydrogen sulfide in novel rat models of non-erosive esophagitis. PLoS One 2014; 9: e110688. |
| 34. | Choi JM, Yang JI, Kang SJ, et al. Association between anxiety and depression and gastroesophageal reflux disease: results from a large cross-sectional study. J Neurogastroenterol Motil 2018; 24: 593-602. |
| 35. | Guadagnoli L, Yadlapati R, Taft T, Pandolfino JE, Tye M, Keefer L. Esophageal hypervigilance is prevalent across gastroesophageal reflux disease presentations. Neurogastroenterol Motil 2021; 33: e14081. |
| 36. |
Woodland P, Shen Ooi JL, Grassi F, et al. Superficial esophageal mucosal afferent nerves may contribute to reflux hypersensitivity in nonerosive reflux disease. Gastroenterology 2017; 153: 1230-9.
DOI PMID |
| 37. |
Savarino E, Coletta MD. Oesophagus: Symptom perception in patients with NERD: do nerves matter? Nat Rev Gastroenterol Hepatol 2017; 14: 634-6.
DOI PMID |
| 38. | Yu M, Chang C, Undem BJ, Yu S. Capsaicin-sensitive vagal afferent nerve-mediated interoceptive signals in the esophagus. Molecules 2021; 26: 3929. |
| 39. | Bastian-Eugenio CE, Bohorquez-Hernandez A, Pacheco J, et al. Heterologous calcium-dependent inactivation of Orai 1 by neighboring TRPV1 channels modulates cell migration and wound healing. Commun Biol 2019; 2:88. |
| 40. | Huang J, Wang Y, Xu P, et al. Molecular mechanism of the effect of zhizhu pill on gastroesophageal reflux disease based on network pharmacology and molecular docking. Evid Based Complement Alternat Med 2022; 2022: 2996865. |
| 41. | Qiu Y, Hu JL, Zhao CC, et al. Zhujie Hewei granules ameliorated reflux esophagitis in rats. Evid Based Complement Alternat Med 2019; 2019: 1392020. |
| 42. | Zhong C, Liu K, Wang K, et al. Developing a diagnostic understanding of GERD phenotypes through the analysis of levels of mucosal injury, immune activation, and psychological comorbidity. Dis Esophagus 2018; 31: doy039. |
| 43. | Han X, Zhang Y, Lee A, et al. Upregulation of acid sensing ion channels is associated with esophageal hypersensitivity in GERD. FASEB J 2022; 36: e22083. |
| 44. | Li YJ, Dai C, Jiang M. Mechanisms of probiotic VSL#3 in a rat model of visceral hypersensitivity involves the mast cell-PAR2-TRPV1 pathway. Dig Dis Sci 2019; 64: 1182-92. |
| 45. | Moore C, Gupta R, Jordt SE, Chen Y, Liedtke WB. Regulation of pain and ich by TRP channels. Neurosci Bull 2018; 34: 120-42. |
| 46. |
Zayachkivska O, Pshyk-Titko I, Hrycevych N, Savytska M. New insight into oseophageal injury and protection in physiologically relevant animal models. J Physiol Pharmacol 2014; 65: 295-307.
PMID |
| [1] | LI Siting, WANG Shaojun, YIN Yehui, DE Gejing, LI Caicai, WANG Ziyan, CAO Wenjie. Electroacupuncture alleviates zymosan-induced colorectal hypersensitivity [J]. Journal of Traditional Chinese Medicine, 2025, 45(1): 32-38. |
| [2] | ZHANG Fang, YAN Cuina, WENG Zhijun, WU Luyi, QI Li, ZHAO Min, XIN Yuhu, WU Huangan, LIU Huirong. Regulatory role of electroacupuncture on satellite glial cell activity in the colon and dorsal root ganglion of rats with irritable bowel syndrome [J]. Journal of Traditional Chinese Medicine, 2024, 44(5): 981-990. |
| [3] | Jiang Jinfeng, Wang Xinjun, Wu Xiaojing, Yu Zhi. Analysis of factors influencing moxibustion efficacy by affecting heat-activated transient receptor potential vanilloid channels [J]. Journal of Traditional Chinese Medicine, 2016, 36(02): 255-260. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||

