Journal of Traditional Chinese Medicine ›› 2022, Vol. 42 ›› Issue (3): 353-363.DOI: 10.19852/j.cnki.jtcm.20220408.002
• Research Article • Previous Articles Next Articles
Correlation between slow transit constipation and spleen Qi deficiency, and gut microbiota: a pilot study
YU Zeyue1, HAO Liyu1, LI Zongyuan2, SUN Jianhui1, CHEN Hongying3, HUO Hairu1, LI Xiaoqin1, SHAN Zhongchao4, LI Hongmei1( )
)
- 1 Institute of Chinese Materia Medica, China Academy of Chinese Medical Sciences, Beijing 100007, China
2 Jiangsu University, Zhenjiang 212013, China
3 Yunnan University of Traditional Chinese Medicine, Kunming 650504, China
4 Jiangxi University of Traditional Chinese Medicine, Nanning 330004, China
-
Received:2021-09-12Accepted:2021-11-17Online:2022-04-08Published:2022-04-08 -
Contact:LI Hongmei -
About author:Pro. LI Hongmei, Institute of Chinese Materia Medica, China Academy of Chinese Medical Sciences, Beijing 100007, China. lihm2006@sina.cn
-
Supported by:Fundamental Scientific Research Business Fees of Central Public Welfare Scientific Research Institutes of China Academy of Chinese Medical Sciences(Z2021022);National Natural Science Foundation Project: Study on the Authenticity of Traditional Chinese Medicine(81891010);Science and Technology Innovation Project of China Academy of Chinese Medical Sciences: Efficacy Evaluation and Mechanism Exploration of Huashi Baidu Granule based on "multi-link and multi-target" in the Prevention and Treatment of Influenza Virus Infection(CI2021A04605);Basic Scientific Research Business Fee Project of Central Public Welfare Scientific Research Institutes of the Chinese Academy of Chinese Medical Sciences: Study on the Novel Coronavirus Pneumonia Mech-anism of Yiqi Zeng Fang and Huashi Baidu Granules(ZZ15-WT-04)
Cite this article
YU Zeyue, HAO Liyu, LI Zongyuan, SUN Jianhui, CHEN Hongying, HUO Hairu, LI Xiaoqin, SHAN Zhongchao, LI Hongmei. Correlation between slow transit constipation and spleen Qi deficiency, and gut microbiota: a pilot study[J]. Journal of Traditional Chinese Medicine, 2022, 42(3): 353-363.
share this article
| Group | Dosage | n | Body weight | |
|---|---|---|---|---|
| Female | Male | |||
| Control | - | 5 | 24.5±2.2 | 31.6±2.2 |
| Model | - | 5 | 20.0±1.2a | 19.7±0.9a |
| MR | 6.24 g/kg | 5 | 19.9±1.8 | 20.4±1.0 |
| Control+ FMT | 200 μL per mouse | 5 | 25.5±2.4 | 33.9±2.9 |
| Model+ FMT | 200 μL per mouse | 5 | 19.7±1.0b | 22.9±1.7b |
| MR+ FMT | 200 μL per mouse | 5 | 18.7±1.8 | 24.1±1.4 |
Table 1 Body weight of female mice which had STC with deficiency of spleen Qi (g, $\bar{x}\pm s$)
| Group | Dosage | n | Body weight | |
|---|---|---|---|---|
| Female | Male | |||
| Control | - | 5 | 24.5±2.2 | 31.6±2.2 |
| Model | - | 5 | 20.0±1.2a | 19.7±0.9a |
| MR | 6.24 g/kg | 5 | 19.9±1.8 | 20.4±1.0 |
| Control+ FMT | 200 μL per mouse | 5 | 25.5±2.4 | 33.9±2.9 |
| Model+ FMT | 200 μL per mouse | 5 | 19.7±1.0b | 22.9±1.7b |
| MR+ FMT | 200 μL per mouse | 5 | 18.7±1.8 | 24.1±1.4 |
| Group | Dosage (g/kg) | n | Time for the first black bowel movement (min) | Number of black stools | Black stools weight (g/6 h) |
|---|---|---|---|---|---|
| Control | - | 10 | 75.50±29.30 | 34.10±6.80 | 0.42±0.10 |
| Model | - | 10 | 139.80±26.80a | 23.60±4.60c | 0.28±0.11e |
| MR | 6.24 | 10 | 74.80±56.00b | 31.90±8.40d | 0.36±0.08 |
Table 2 Fecal parameters measurement of mice which had STC with deficiency of spleen Qi ($\bar{x}\pm s$)
| Group | Dosage (g/kg) | n | Time for the first black bowel movement (min) | Number of black stools | Black stools weight (g/6 h) |
|---|---|---|---|---|---|
| Control | - | 10 | 75.50±29.30 | 34.10±6.80 | 0.42±0.10 |
| Model | - | 10 | 139.80±26.80a | 23.60±4.60c | 0.28±0.11e |
| MR | 6.24 | 10 | 74.80±56.00b | 31.90±8.40d | 0.36±0.08 |
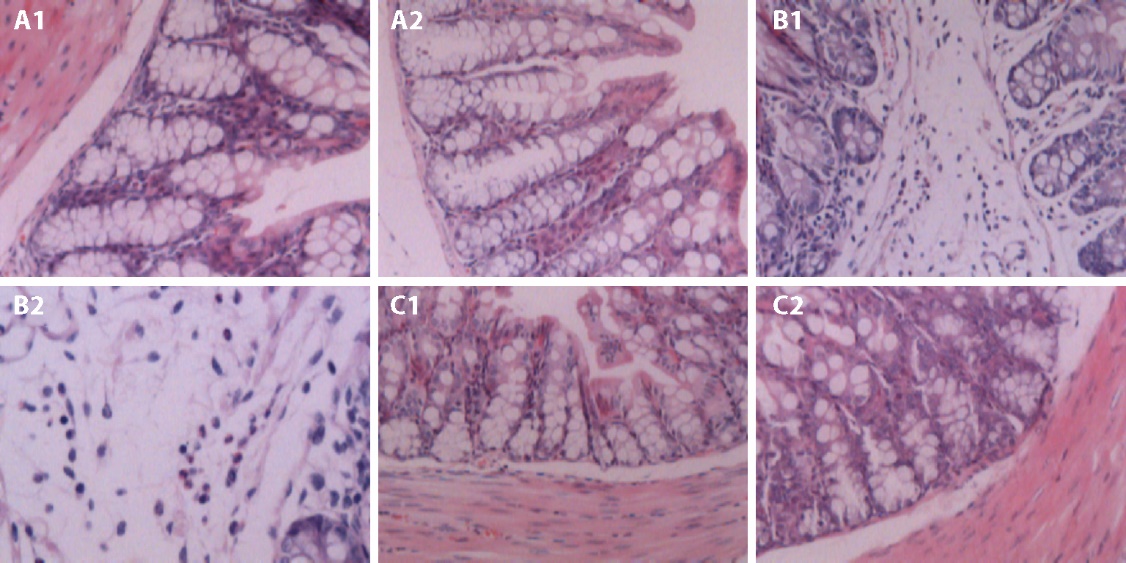
Figure 1 HE staining to observe the pathological changes and characteristics of colon tissue and inflammatory cell infiltration in mice A-C: hematoxylin-eosin (HE) staining of colon tissue (× 200). A-C: pathological changes of control group, model group, MR group. A1, A2: control group: normal mice without treatment (n = 10); B1, B2: model group: Slow transit constipation with deficiency of spleen Qi mice without treatment (n = 10); C1, C2: MR group: Slow transit constipation with deficiency of spleen Qi mice with Maren Runchang pills intragastrically at a daily dose of 6.24 g/kg (n = 10).
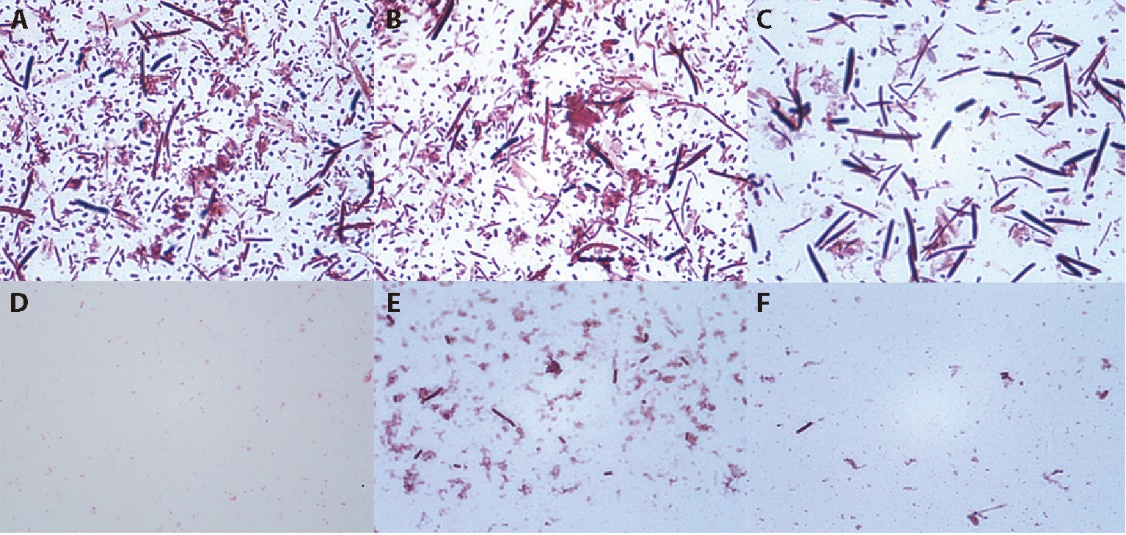
Figure 2 Evaluation index of pseudo germfree mice A-F: direct fecal smear and gram stain method (× 400). A-C: fecal of normal mice (n = 10), there were lots of gram-negative bacteria (blue) and gram-positive bacteria (red); D-F: fecal of pseudo germfree mice which prepared by gavaging combined antibiotics for 7 days (n = 30), there were hardly any gram-negative bacteria (blue) and gram-positive bacteria (red).
| Group | Dosage | n | SP content | VIP content |
|---|---|---|---|---|
| Control | - | 10 | 0.45±0.08 | 0.60±0.13 |
| Model | - | 10 | 0.32±0.05a | 0.80±0.27e |
| Mr | 6.24 g/kg | 10 | 0.44±0.11b | 0.57±0.19f |
| Control+ FMT | 200 μL per mouse | 10 | 0.42±0.09 | 0.50±0.11 |
| Model+ FMT | 200 μL per mouse | 10 | 0.35±0.04c | 0.65±0.25 |
| Mr+ Fmt | 200 μL per mouse | 10 | 0.42±0.10d | 0.47±0.04g |
Table 3 The SP, VIP content of mice which had STC with deficiency of spleen Qi in 5 % colon homogenate (pg/mg, $\bar{x}\pm s$)
| Group | Dosage | n | SP content | VIP content |
|---|---|---|---|---|
| Control | - | 10 | 0.45±0.08 | 0.60±0.13 |
| Model | - | 10 | 0.32±0.05a | 0.80±0.27e |
| Mr | 6.24 g/kg | 10 | 0.44±0.11b | 0.57±0.19f |
| Control+ FMT | 200 μL per mouse | 10 | 0.42±0.09 | 0.50±0.11 |
| Model+ FMT | 200 μL per mouse | 10 | 0.35±0.04c | 0.65±0.25 |
| Mr+ Fmt | 200 μL per mouse | 10 | 0.42±0.10d | 0.47±0.04g |
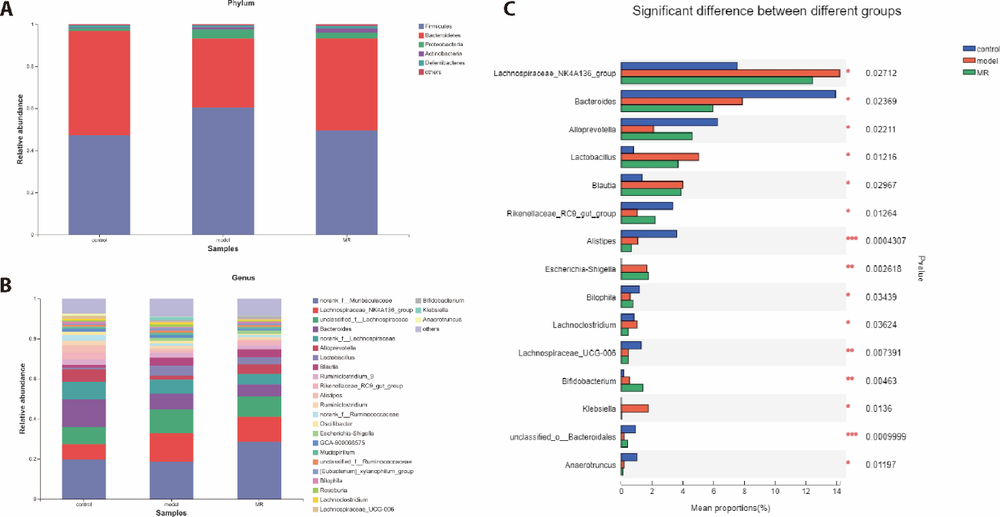
Figure 3 Significant difference of relative abundance of gut microbiota in slow transit constipation mice====A-C: described relative abundance of gut microbiota at the phylum and genus level respectively, which could present 2 aspects of information intuitively: which dominant species were contained in each sample at a given taxonomic level, and the relative abundance (proportion of the sample) of each dom89*9inant species.
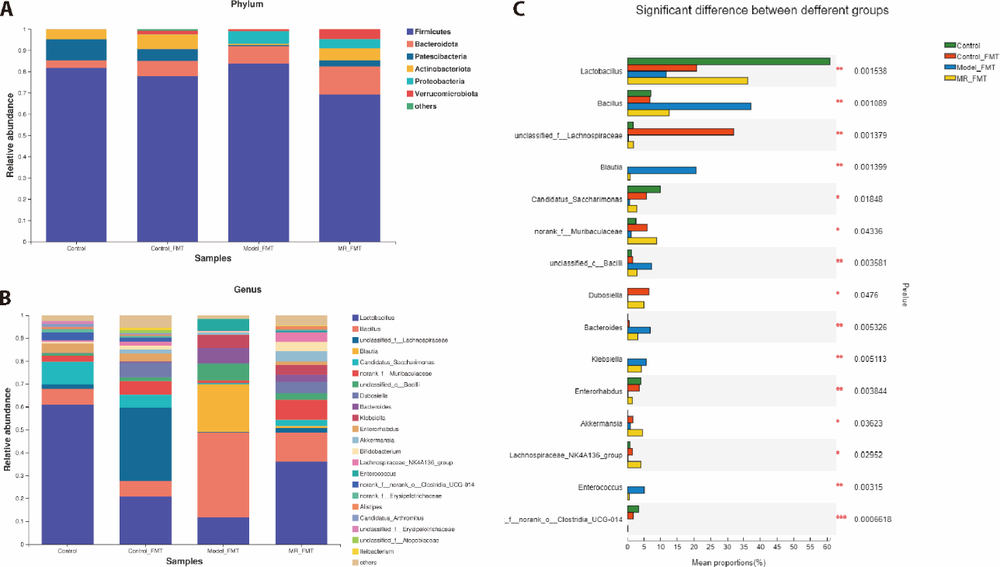
Figure 4 Relative abundance of gut microbiota in pseudo germfree mice A-C: described relative abundance of gut microbiota at the phylum and genus level respectively, which could present 2 aspects of information intuitively: which dominant species were contained in each sample at a given taxonomic level, and the relative abundance (proportion of the sample) of each dominant species.
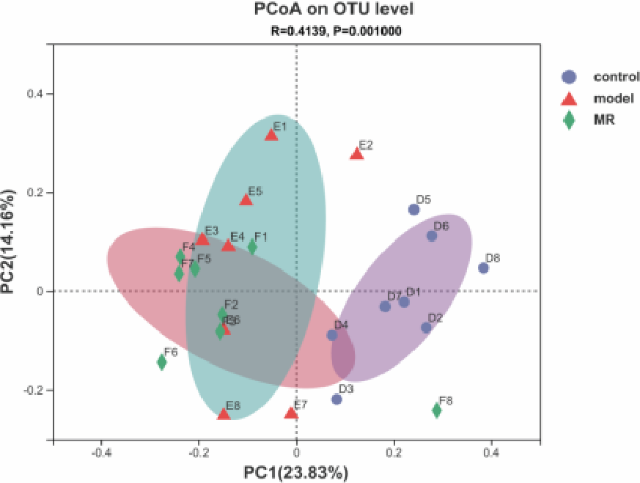
Figure 5 Principal co-ordinates analysis at operational taxonomic unit (OTU) level of slow transit constipation with deficiency of spleen Qi mice P = 0.001 and R = 0.4139 for control, model, MR groups. The points with different shapes and colors in the figure represented samples in different groups. The distance between samples in the same group represented the repeatability of this group of samples; The distance of samples between different groups represented the difference between different groups.
| Group | R value | P value |
|---|---|---|
| Control & Model | 0.2018 | 0.001 |
| Model & MR | 0.1024 | 0.044 |
| Control & Model& MR | 0.2321 | 0.001 |
Table 4 PerMANOVA analysis results between different groups at OTU level of slow transit constipation with deficiency of spleen Qi mice
| Group | R value | P value |
|---|---|---|
| Control & Model | 0.2018 | 0.001 |
| Model & MR | 0.1024 | 0.044 |
| Control & Model& MR | 0.2321 | 0.001 |
| Group | R value | P value |
|---|---|---|
| Control + FMT & model + FMT | 0.5012 | 0.006 |
| Model + FMT& MR + FMT | 0.5498 | 0.007 |
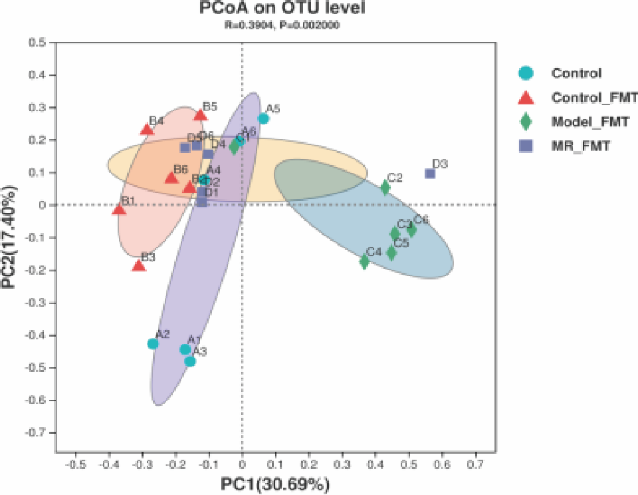
| control + FMT& model + FMT& MR + FMT | 0.3904 | 0.002 |
Table 5 PerMANOVA analysis results between different groups at OTU level of pseudo germfree mice
| Group | R value | P value |
|---|---|---|
| Control + FMT & model + FMT | 0.5012 | 0.006 |
| Model + FMT& MR + FMT | 0.5498 | 0.007 |
| control + FMT& model + FMT& MR + FMT | 0.3904 | 0.002 |
| 1 | Wang WS, Xia XT, Liu FL, et al. Effects of Zhizhu pills on intestinal motility and PLC-γ_1/PLC-γ_2 signal pathway in mice with slow transit constipation of spleen deficiency syndrome. Zhong Guo Shi Yan Fang Ji Xue Za Zhi 2019; 25:8-14. |
| 2 |
Eor J Y, Tan P L, Lim S M, et al. Laxative effect of lotte probiotic chocolat on loperamide-induced constipation in rats. Food Res Int 2018; 116:1173-82.
DOI URL |
| 3 |
Black CJ, Ford AC. Chronic idiopathic constipation in adults: epidemiology, pathophysiology, diagnosis and clinical management. Med J Aust 2018; 209:86-91.
DOI URL |
| 4 |
Jiang H, Dong J, Jiang S, et al. Effect of durio zibethinus rind polysaccharide on functional constipation and intestinal microbiota in rats. Food Res Int 2020; 136:109316.
DOI URL |
| 5 |
Dinning P G, Lorenzo C D. Colonic dysmotility in constipation. Best Pract Res Clin Gastroenterol 2011; 25:89-101.
DOI PMID |
| 6 | Wu MH, Wang XY. Zhong Yi Nei Ke Xue. Beijing: China Press of Traditional Chinese Medicine, 2012; 237-8. |
| 7 | Zhang JY (Ming dynasty). Jing Yue Quan Shu. Beijing: People's Medical Publishing House, 2007: 540. |
| 8 | Li DY (Yuan dynasty). Pi Wei Lun. Beijing: People's Medical Publishing House, 2005: 92. |
| 9 | Tan ZR, Tan L, Huang X, et al. Changes of interstitial cells of Cajal in the colon of rats with slow transit constipation. Shi Yong Yi Xue Za Zhi 2011; 27:3290-2. |
| 10 |
Boeckxstaens G, Camilleri M, Sifrim D, et al. Fundamentals of neurogastroenterology: physiology/motility-sensation. Gastroenterology 2016; 150:1292-304.
DOI URL |
| 11 |
Obata Y, Pachnis V. The Effect of microbiota and the immune system on the development and organization of the enteric nervous system. Gastroenterology 2016; 151:836-44.
DOI URL |
| 12 |
Zhao Y, Yu YB. Intestinal microbiota and chronic constipation. Springerplus 2016; 5:1130.
DOI URL |
| 13 |
Zhu LX, Liu WS, Alkhouri R, et al. Structural changes in the gut microbiome of constipated patients. Physiol Genomics 2014; 46:679-86.
DOI URL |
| 14 | Choi C H, Chang S K. Alteration of gut microbiota and efficacy of probiotics in functional constipation. JNM 2015; 21:4-7. |
| 15 |
Parthasarathy G, Chen J, Chen XF, et al. Relationship between microbiota of the colonic mucosa vs feces and symptoms, colonic transit, and methane production in female patients with chronic constipation. Gastroenterology 2016; 150:367-79.
DOI PMID |
| 16 | Nunes N S, Kim S, Sundby M, et al. Temporal clinical, proteomic, histological and cellular immune responses of dextran sulfate sodium-induced acute colitis. WJG 2018; 24:4341-55. |
| 17 |
Wei YL, Chen YQ, Gong H, et al. Fecal microbiota transplantation ameliorates experimentally induced colitis in mice by upregulating AhR. Front Microbiol 2018; 9:19-21.
DOI URL |
| 18 |
Magoc T, Salzberg S L. FLASH: fast length adjustment of short reads to improve genome assemblies. Bioinformatics 2011; 27:2957-63.
DOI URL |
| 19 | Edgar R C. UPARSE: highly accurate OTU sequences from microbial amplicon reads. Nat Methods 2013; 10: 996-8. |
| 20 | Wang Q, Garrity G M, Tiedje J M, Cole J R. Naive bayesian classifier for rapid assignment of rRNA sequences into the new bacterial taxonomy. Appl Environ Microbiol 2007; 73: 5261-7. |
| 21 | Tian JX, Lai QK, Ma ZC, et al. The effect of Fuxiekang on immunity, digestion and absorption in rats with spleen deficiency and diarrhea syndrome. Zhong Guo Lin Chuang Kang Fu 2006; 10:92-4. |
| 22 | Zhu SD, Li BP, Qiao Q. Effect of Yunmu powder on amylase and xylose in rats with spleen deficiency and diarrhea. Zhe Jiang Zhong Yi Yao Da Xue Xue Bao 2002; 26:46-7. |
| 23 | Pang X, Liu YQ, Liu XD. The effect of different parts of atractylodes japonicus with bran on spleen deficiency in rats. Xian Dai Yao Wu Yu Lin Chuang 2015; 30:763-7. |
| 24 | Sun XZ, Ma ZQ, Ma XQ. A preliminary study on the relationship between VIP, substance P and constipation. Shi Jie Zui Xin Yi Xue Xin Xi Wen Zhai 2019; 19:113-4. |
| 25 |
Long LL, Wang JN, Chen NN, et al. Curcumin ameliorates reserpine-induced gastrointestinal mucosal lesions through inhibiting IκB-α/NF-κB pathway and regulating expression of vasoactive intestinal peptide and gastrin in rats. J Med Food 2016; 19:528-34.
DOI URL |
| 26 | Zhu F, Xu S, Zhang Y, et al. Total glucosides of paeony promote intestinal motility in slow transit constipation rats through amelioration of interstitial cells of Cajal. Plos One 2016; 11. |
| 27 | Chen R, Zhou BY, Zhou L. Effects of atractylodes macrocephala on enteric neurotransmitter and ICC in mice with slow transit constipation. Chong Qing Yi Ke Da Xue Xue Bao 2022; 47:1-8. |
| 28 |
Ley RE, Turnbaugh PJ, Klein S, et al. Microbial ecology: human gut microbes associated with obesity. Nature 2006; 444:1022-3.
DOI URL |
| 29 |
Turnbaugh P J, Hamady M, Yatsunenko T, et al. A core gut microbiome in obese and lean twins. Nature 2009; 457:480-4.
DOI URL |
| 30 | Dong KZ, Fu SW, Sheng L, et al. The effect of Cordyceps sinensis mycelium on serum VIP and SP in mice with intestinal microflora disorders. Jie Fang Jun Yi Xue Za Zhi 2014; 11:873-6. |
| 31 |
Salinas C J, Cavazzuti A, et al. Therapeutic efficacy of stable analogues of vasoactive intestinal peptide against pathogens. J Biol Chem 2014; 289:14583-99.
DOI URL |
| 32 | Cong LM, Dong WW, Jie A, et al. Probiotics combined with dietary fiber to improve constipation. Zhong Guo Wei Sheng Tai Xue Za Zhi 2016; 06:632-8. |
| 33 |
Radka CD, Frank MW, Rock CO, et al. Fatty acid activation and utilization by Alistipes finegoldii, a representative Bacteroidetes resident of the human gut microbiome. Mol Microbiol 2020; 113:807-25.
DOI URL |
| 34 |
Eckburg PB, Bik EM, Bernstein CN, et al. Diversity of the human intestinal microbial flora. Science 2005; 308, 1635-8.
DOI PMID |
| 35 | Chen Q, Wu JP, Dong X, et al. Gut flora-targeted photobiomodulation therapy improves senile dementia in an A-induced Alzheimer's disease animal model. J Photochem Photobiol B 2021; 112152. |
| 36 |
Kojima A, Nakano K, Wada K, et al. Infection of specific strains of streptococcus mutans, oral bacteria, confers a risk of ulcerative colitis. Sci Rep 2012; 2:332.
DOI URL |
| 37 |
Liu J, Gao Y, Zhou J, et al. Changes in serum inflammatory cytokine levels and intestinal flora in a self-healing dextran sodium sulfate-induced ulcerative colitis murine model. Life Sci 2020; 263:118587.
DOI URL |
| 38 |
Wu GD, Chen J, et al. Linking long-term dietary patterns with gut microbial enterotypes. Science 2011; 334:105-8.
DOI URL |
| 39 |
Kang D W, Park J G, Ilhan Z E, et al. Reduced incidence of Prevotella and other fermenters in intestinal microflora of autistic children. PLoS One 2013; 8:e68322.
DOI URL |
| 40 | Backhed F, Ding H, Wang T, et al. The gut microbiota as an environmental factor that regulates fat storage. Proc Natl Acad Sci USA 2004; 101.44:15718-23. |
| 41 | Feng CN, Zeng LZ, Wang SJ. Analysis of micro-inflammation and gut microbial diversity in patients with type 2 diabetes and diabetic nephropathy. Zhong Guo Wei Sheng Tai Xue Za Zhi 2020; 32:1273-78. |
| 42 |
Chen YF, Yang FL, Lu HF, et al. Characterization of fecal microbial communities in patients with liver cirrhosis. Hepatology 2011; 54:562-72.
DOI URL |
| 43 | Manuel CR, Latuga MS, Ashby CR, et al. Immune tolerance attenuates gut dysbiosis, dysregulated uterine gene expression and high-fat diet potentiated preterm birth in mice. Am J Obstet Gynecol 2019; 220, 596.e1-28. |
| 44 |
Peck SC, Denger K, Burrichter A, et al. A glycyl radical enzyme enables hydrogen sulfide production by the human intestinal bacterium bilophila wadsworthia. Proc Natl Acad Sci USA 2019; 116:3171-6.
DOI URL |
| 45 |
Herridge WP, Shibu P, et al. Bacteriophages of klebsiella spp., their diversity and potential therapeutic uses. J Med Microbiol 2020; 69:176-94.
DOI PMID |
| 46 |
Liu Q, Cai BY, Zhu LX, et al. Liraglutide modulates gut microbiome and attenuates nonalcoholic fatty liver in db/db mice. Life Sci 2020; 261:118457.
DOI URL |
| 47 |
Koh A, Vadder DF, Datchary KP, et al. From dietary fiber to host physiology: short-chain fatty acids as key bacterial metabolites. Cell 2016; 165:1332-45.
DOI URL |
| 48 |
Dong CR, Yu JQ, Yang YN, et al. Berberine, a potential prebiotic to indirectly promote Akkermansia growth through stimulating gut mucin secretion. Biomed Pharmacother 2021; 139:111595.
DOI URL |
| [1] | LI Chaoran, YANG Yan, FENG Chuwen, LI Heng, QU Yuanyuan, WANG Yulin, WANG Delong, WANG Qingyong, GUO Jing, SHI Tianyu, SUN Xiaowei, WANG Xue, HOU Yunlong, SUN Zhongren, YANG Tiansong. Integrated 'omics analysis for the gut microbiota response to moxibustion in a rat model of chronic fatigue syndrome [J]. Journal of Traditional Chinese Medicine, 2023, 43(6): 1176-1189. |
| [2] | ZHOU Jun, WANG Junhua, LI Xiaobing, WAN Chenyi, LI Fangjun, Lü Yanni, CHEN Hao, SUN Meiying. Efficacy of Heshouwu (Radix Polygoni Multiflori) on gut mircobiota in mice with autoimmune encephalomyelitis [J]. Journal of Traditional Chinese Medicine, 2023, 43(4): 676-685. |
| [3] | JIANG Yiqian, ZHOU Xibin, PU Wenyuan, ZHOU Chunxiang. Sanwu Baisan decoction (三物白散) inhibits colorectal cancer progression in mice by remodeling gut microbiota and tumorigenesis [J]. Journal of Traditional Chinese Medicine, 2023, 43(3): 466-473. |
| [4] | YANG Yang, YUAN Haining, JIA Hongxiao, NING Yanzhe, WANG Di, ZHANG Lei, YAN Kaijuan, GUO Yumeng, WANG Fei, SUN Weishuang, CHEN Pei. Therapy of replenishing Yin and regulating Yang for manic episode in bipolar disorder: study protocol for a prospective, double-blind, randomized controlled trial [J]. Journal of Traditional Chinese Medicine, 2023, 43(3): 594-601. |
| [5] | SUN Mengzhu, ZHANG Yujie, SONG Yafang, GUO Jing, ZHAO Tingting, WANG Yuhang, PEI Lixia, SUN Jianhua. Electroacupuncture at Tianshu (ST25) and Zusanli (ST36) alleviates stress-induced irritable bowel syndrome in mice by modulating gut microbiota and corticotropin-releasing factor [J]. Journal of Traditional Chinese Medicine, 2022, 42(5): 732-740. |
| [6] | Huixiang ZHANG, Limei WANG, Jipeng GUO, Jiai WANG, Qianqian ZHANG, Yutao WANG, Xun LIU, Lihuan ZHANG, Lanlan SHI, Hongxiang WU, Xue CAO. Gut microbiota and differential genes-maintained homeostasis is key to maintaining health of individuals with Yang-deficiency constitution [J]. Journal of Traditional Chinese Medicine, 2022, 42(1): 96-101. |
| [7] | PAN Lijia, MA Shuya, WEN Jing, ZHANG Xiaoqi, XING Haijiao, JIA Chunsheng. Direct contact moxibustion promotes apoptosis of gastric cancer cells in rats by regulating intestinal flora [J]. Journal of Traditional Chinese Medicine, 2021, 41(6): 943-952. |
| [8] | Gao Lujiao, Niu Xin, Niu Tingli, Wang Xuan, Lu Xiaoyan, Feng Qianjin, Yang Xuezhi. Curative efficacy of extract from Ganjiangdazao recipe on functional dyspepsia in rats [J]. Journal of Traditional Chinese Medicine, 2020, 40(4): 654-663. |
| [9] | Sun Zhigao, Hu Yazhuo, Wang Yuguo, Feng Jian, Dou Yongqi. Bupi Hewei decoction ameliorates 5-fluorouracil-induced intestinal dysbiosis in rats through T helper 17/T regulatory cell signaling pathway [J]. Journal of Traditional Chinese Medicine, 2020, 40(1): 38-48. |
| [10] | Peng Ying, Zhang Shuoying, Liu Zhiwei, Ji Jia, Wu Chunfu, Yang Jingyu, Li Xiaobo. Gut microbiota and Chinese medicine syndrome: altered fecal microbiotas in spleen(Pi)-deficient patients [J]. Journal of Traditional Chinese Medicine, 2020, 40(1): 137-143. |
| [11] | Wang Yingying, Xu Dongsheng, Bai Wanzhu, Yang Jinsheng. Effects of Guasha on histomorphology of scraped skins and on expression of calcitonin gene-related peptide and substance P in rats [J]. Journal of Traditional Chinese Medicine, 2018, 38(04): 562-569. |
| [12] | Lu Zhenzhong, Yin Xiaojun, Teng Weijun, Chen Yuehua, Sun Jie, Zhao Jimeng, Wang Anqi, Bao Chunhui, Shi Yin. Comparative effect of electroacupuncture and moxibustion on the expression of substance P and vasoactive intestinal peptide in patients with irritable bowel syndrome [J]. Journal of Traditional Chinese Medicine, 2015, 35(04): 402-410. |
| [13] | Hu Rui , Tang Fang. Effects of Wei Chang An pill(胃肠安丸) on enzyme activity and levels of vasoactive peptide and substance P in the small intestine of rats with compound diarrhea [J]. Journal of Traditional Chinese Medicine, 2012, 32(01): 52-57. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||